Oesophageal Detector Devices
Dr RP Haridas,
Lecturer & Professor DA Rocke, Department of Anaesthetics, Faculty of Medicine, University of Natal, Private Bag 7, Congella, 4013 Durban, South Africa.
fax: (31) 260 4433 e-mail : haridas@med.und.ac.za
|
||
|
Introduction
Oesophageal intubation may occur with a difficult laryngoscopy, inexperience, an emergency situation, accidental extubation with movement of the patient's head, or distraction of the person intubating. An unrecognized oesophageal intubation may result in gastric distension, regurgitation, and hypoxic damage to the brain. Early detection of oesophageal intubation will prevent or reduce the morbidity and mortality of this life threatening situation. There are both clinical and technical tests that can be used to assess tracheal tube position 1. Occasionally clinical tests prove unreliable and confirmation of the correct placement of the endotracheal tube by technical means is useful. One of the simplest and most reliable methods involves the use of an oesophageal detector device (ODD), the best alternative to capnography in differentiating oesophageal from tracheal intubation.
Although usually referred to as an ODD, both oesophageal and tracheal intubations are detected and due to its method of operation it has also been termed the negative pressure device.
Oesophageal detector devices (ODD) are designed to aspirate air via the endotracheal tube and depend on the structural differences between the trachea and oesophagus to indicate ETT position. The ability to aspirate air easily when connected to an ETT indicates tracheal intubation as the trachea and main bronchi have a rigid structure and do not collapse when a negative pressure is applied. Failure to aspirate air indicates oesophageal intubation as the oesophagus collapses around the end of the ETT. ![]()
Types of oesophageal detector devices
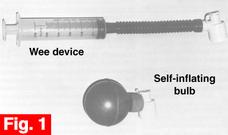
There are two major types of ODD (Figure 1). The first ODD was described in 1980 2, but Wee (1988) was the first to use the term oesophageal detector device, and also the first to publish a study on it 3. |
|
The ODD is made by connecting a 60 ml catheter-tip syringe to a right-angled endotracheal tube connector by a short length of rubber tubing (Figure 1). The device is attached to an ETT and the syringe aspirated. If resistance is encountered when the syringe is aspirated i.e. with an oesophageal intubation, when the plunger is released it usually rebounds to its original position. O'Leary 4 regarded the aspiration of 30mls of air as indicating tracheal intubation.
Nunn described an adaptation using an Ellick's evacuator (a rubber bulb) and a connector 5. The bulb is squeezed and attached to the ETT. Passive re-inflation indicates a tracheal intubation, while a failure to reinflate occurs with an oesophageal intubation. The bulb from a disposable bulb syringe may also be used.
The advantages of the ODD are listed in ![]() table 1.
table 1.
- ODDs can be easily assembled using inexpensive and readily available equipment. They are easy to use (even by non-anaesthetists), portable, non-electronic, and provide a highly reliable assessment of ETT position. They are ideal for use in countries where capnography is not routinely available. They may also be useful for intubations performed outside the operating room (e.g., in the recovery room, emergency room, intensive care unit, and out in the field).
- ODDs provide a rapid assessment of ETT position. In Wee's original study 3, the average time to perform the test was 6.9 seconds (range 5 - 16 seconds). Nunn 5 obtained a result with the Ellick's bulb in 3 - 5 seconds. When the bulb from a disposable bulb syringe was used, full re-inflation of the bulb took up to 30 seconds in only 6% of tracheal intubations 6. The result of the ODD test is obtained more rapidly than that from capno-graphy, and relies solely on observation.
- ODDs are useful in patients in cardiac arrest as the test result does not depend on carbon dioxide being present in exhaled gas.
- ODDs are useful when a Combitube (an emergency device that can be inserted into the airway blindly and used to ventilate patients) has been used. They can indicate whether the Combitube is positioned in the trachea or oesophagus, and whether or not the airway is patent.
- ODDs can be re-used after cleaning or sterilisation.
The disadvantages of the ODD include:
- Some false results may occur (
 Table 2). However, the incidence of this is low.
Table 2). However, the incidence of this is low. - Regurgitation of gastric air, distension of the oesophagus with air, or an ODD that is not airtight may give a false impression of tracheal intubation when the tube is in fact in the oesophagus.
- Thick secretions may occlude a tracheal tube 3 and give a false impression of oesophageal intubation. Occlusion of the bevel of a reinforced ETT by the wall of the trachea has been described to cause failure of bulb refill. Bronchial intubation, bronchospasm, tracheal compression, obesity, chronic obstructive pulmonary disease, may also cause resistance to aspiration or delayed refill of the bulb-type ODD.
- Wee 3 had no problem in identifying tracheal intubation in two patients with moderate broncho-spasm (peak airway pressures of 3.0 - 4.2kPa). However, delayed refill of the bulb-type ODD has been observed in an asthmatic patient. The slow re-inflation of the bulb seen in the presence of bronchospasm represents the slow exhalation that is characteristic of acute asthma.
![[Top]](../../../../clip_image002_0000.gif)
Conclusions: role of the ODD
The ODD is a simple device, and its underlying principle is easy to explain, even to non-anaesthetists. Wee stated that instruction on the use of his device took five minutes. The ODDs have been reliably used by paramedics and by doctors not trained in anaesthesia.
ODDs are inexpensive, easily assembled, and generally very reliable. Although the required components may be found in many operating rooms it will take several minutes, at the very least, to collect and assemble them. The ODD should, therefore, be preassembled.
ODDs are ideal for use where capnography is unavailable. They are useful in hospitals which have capnography in the operating theatres, but not in the recovery rooms, wards and emergency rooms, and in hospitals where capnography is not yet available or affordable. It must be stressed that ODDs do not replace capnography, but they are the best alternative method to capnography in differentiating oesophageal from tracheal intubation. The ODDs must not be used on their own, but always in conjunction with clinical methods to assess endotracheal tube position. ![]()
References
A copy of this article with a full set of references can be obtained by writing or sending e-mail to Dr.R.P. Haridas.
- Clyburn P, Rosen M. "Accidental oesophageal intubation." (Review) British Journal of Anaesthesia 1994; 73: 55-63.
- Pollard B. "Oesophageal detector device." (Letter) Anaesthesia 1988; 43: 713-4.
- Wee MYK. "The oesophageal detector device. Assessment of a new method to distinguish oesophageal from tracheal intubation." Anaesthesia 1988; 43: 27-29.
- O'Leary JJ, Pollard BJ, Ryan MJ. " A method of detecting oesophageal intubation or confirming tracheal intubation." Anaesthesia and Intensive Care 1988; 16: 299-301.
- Nunn JF. "The oesophageal detector device." (Letter) Anaesthesia 1988; 43: 804.
- Zaleski L, Abello D, Gold MI. "The esophageal detector device. Does it work?" Anesthesiology 1993; 79: 244-7.